If you’re considering breast reduction surgery, it’s natural to wonder how long recovery takes and what healing really involves. This guide covers what to expect—from the first 48 hours to long-term recovery—and offers practical tips to help you heal faster, stay comfortable, and get back to daily life with confidence.
While everyone heals at their own pace, understanding the recovery process can make a big difference. We’ll walk you through the key milestones, address common concerns, and share advice to support your journey from day one.
How Long Does Breast Reduction Recovery Take?
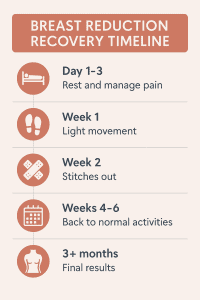
Recovery after breast reduction surgery happens in phases:
- First 1–2 weeks: Most discomfort and swelling occur during this time. You’ll need to rest, take pain medications as prescribed, and wear a support bra.
- Weeks 2–6: Swelling and bruising improve. Many patients return to light activities or work by week 2. More strenuous movement and exercise are still limited.
- After 6 weeks: Most physical restrictions are lifted. Final breast shape and scar appearance continue to improve over the coming months.
- Full recovery: It can take up to 6–12 months for all swelling to resolve and scars to fade.
Every person heals differently, but following your surgeon’s advice and giving your body time will lead to the best results.
First 24–48 Hours After Surgery
The first couple of days after surgery are all about rest and support. Here’s what to expect:
- Pain & swelling: These are at their peak in the first 48 hours. Take prescribed pain medication and keep your upper body elevated to reduce discomfort.
- Limited movement: Avoid lifting your arms, bending, or walking too much. Have a friend or family member help you with meals, medication, and bathroom trips.
- Wound care: Your breasts will be bandaged or wrapped. Follow your surgeon’s instructions for dressing care and do not remove anything unless advised.
- No showering: Most surgeons recommend sponge baths only during this time. Keep the incision area clean and dry.
- Stay hydrated & eat light: Sip water frequently and eat small meals to avoid nausea. Avoid alcohol and smoking completely.
Being prepared and taking it slow during this critical period helps lay the foundation for a smoother, easier recovery ahead.
Week 1: Rest, Support & Gentle Movement
After the first 48 hours, most patients start to feel a bit more mobile—but this is still a time for rest and careful movement.
- Pain management: You may start tapering off stronger painkillers after a few days. Switch to paracetamol or ibuprofen if approved by your surgeon.
- Support bra: Continue wearing your surgical or post-op bra 24/7 to reduce swelling and support healing.
- Gentle walking: Light movement (e.g., walking around the house every hour or two) is encouraged to improve circulation and reduce the risk of blood clots.
- Sleep position: Sleep on your back with your upper body elevated to help reduce swelling and pressure on your incisions.
- Wound care & check-up: Keep your incisions clean and dry. Your first post-op appointment typically happens around day 5–7 to monitor healing and remove any dressings or drains.
Avoid lifting anything heavier than a few pounds, including pets, bags, or children. Listen to your body—fatigue is normal, and overexertion can delay healing.
Weeks 2–3: Light Activity & Early Healing
You’ll likely notice steady improvement in pain, swelling, and mobility.
- Back to work: If your job is not physically demanding, you may feel ready to return around week 2.
- Stitches & scar care: If you have non-dissolvable stitches, they may be removed around this time. Your surgeon may also advise starting silicone gel or sheets to improve scar healing.
- Improved mobility: Light household tasks are usually safe now, but avoid stretching, lifting, or high-impact movement.
- Emotional ups & downs: It’s normal to feel tired or emotional. Hormones, anaesthesia, and post-surgical stress can contribute. Stay in touch with supportive people and don’t hesitate to reach out to your surgical team with questions.
This is a great time to focus on balanced meals, hydration, and daily gentle movement—all of which help speed up healing.

Weeks 4–6: Regaining Confidence & Strength
By now, you’re likely feeling much more like yourself.
- Swelling continues to reduce: Most visible swelling and bruising will have subsided.
- Exercise: Your surgeon may allow low-impact workouts like walking, gentle cycling, or stretching. Avoid chest-focused exercises until cleared.
- Bra options: You may transition to a soft, wireless sports bra if approved. Avoid underwires until your scars are fully healed.
- Side sleeping: Many patients can sleep on their side again around week 6. Continue using pillows for comfort as needed.
- Daily life: Most women resume normal activities with minimal discomfort, including driving, errands, and social outings.
This period often brings a boost in mood as your new breast shape becomes more visible and you return to your routine.
After 6 Weeks: Long-Term Healing & Final Results
You’re entering the final stages of healing, but there’s still internal recovery happening beneath the surface.
- Exercise freedom: In most cases, you can now resume all physical activity—including high-impact workouts—with surgeon approval.
- Scar maturity: Scars will still be visible but should start fading. Continue applying silicone products and protecting scars from sun exposure.
- Breast shape settling: Your breasts may still feel slightly firm or numb in areas. Over the next few months, they’ll soften and continue to take their final shape.
- Emotional adjustment: You may still be adjusting to your new appearance. Give yourself time to mentally and emotionally process the changes.
Most patients are thrilled with their results at this stage, especially as clothing fits better and physical discomfort has improved.
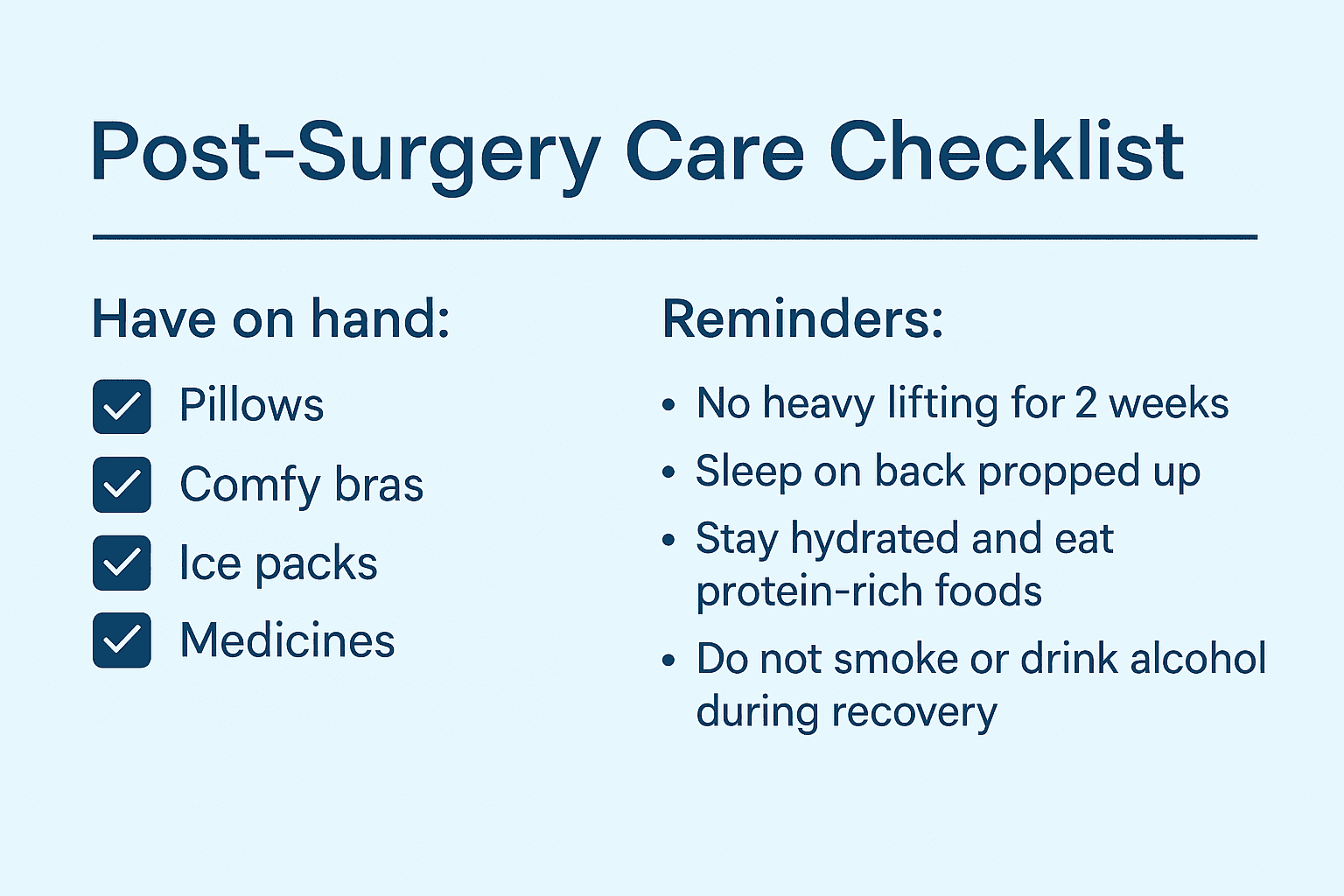
Helpful Recovery Tips
Here are a few simple but powerful tips to support your healing:
- Hydrate & eat well: Protein-rich foods and plenty of water help rebuild tissue and reduce swelling.
- Stick to your follow-ups: Your surgeon will monitor healing and offer tailored advice as you progress.
- Avoid smoking & alcohol: Both can slow healing and affect scar quality.
- Keep a recovery log: Track your meds, symptoms, and progress—it helps you stay organised and gives your surgeon helpful info.
- Be patient: Full healing takes time. Don’t rush the process or compare yourself to others.
When to Contact Your Surgeon
Call your surgeon immediately if you notice:
- Sudden increase in swelling or pain on one side
- Fever over 38°C (100.4°F)
- Redness spreading around incisions
- Yellow or foul-smelling drainage
- Shortness of breath or chest pain
It’s always better to check in than wait if something doesn’t feel right.
Final Thoughts
Breast reduction recovery is a journey, but with the right care and mindset, most women find it completely worthwhile. Take it one week at a time, follow your surgeon’s advice, and allow yourself the time and space to heal—physically and emotionally.
You’re doing something incredibly positive for your body and quality of life. Rest, recover, and look forward to the freedom and comfort ahead.
London Cosmetic Surgery group Berkeley Square Medical, is one of the UK’s leading providers of Aesthetic and Cosmetic Surgery .
For more information about Breast Reduction at Berkeley Square Medical, please visit: https://www.berkeleysquaremedical.com/breast-reduction
Sanjay is a Senior Clinical Member at Berkeley Square Medical carrying over a decade of experience. He has assisted over 1500 surgeries carried out at the hospital supporting patients both pre and post-surgery throughout their treatment journeys. This article was written with the contribution of
Dr Taimur Shoaib, our Consultant Plastic Surgeon.
Latest posts by Sanjay Rai
(see all)
Sharing is caring!
