Revision rhinoplasty aims to correct an undesired aesthetic appearance of your nose caused by a previous Rhinoplasty surgery.
Revision Rhinoplasty is a delicate procedure requiring one of the highest levels of specialisation from your Rhinoplasty Surgeon.
Revision Rhinoplasty is one of the highest inquiries by patients in the cosmetic surgery sector for corrective surgery.
Let’s look at why this growing trend is happening and what you should consider before undergoing a revision rhinoplasty.
REVISION RHINOPLASTY COST IN LONDON
£9950.00
At Berkeley Square Medical, the cost of Revision Rhinoplasty is set at £9950.00. This is an All-Inclusive set price for all Revision Rhinoplasty patients and includes the full cost of your procedure and your £100 consultation, which is credited against the cost of your surgery. All Appointments and Aftercare Treatment are covered within your Aftercare Policy
The cost of your surgery includes the following:
 | Your Full Consultation:£100.00 (Set Fee) Creditable Towards Your Set Surgery Fee Included With Consultation Summary E-Letter. |  | TWO (2) Surgeon Consultations:1st – In-Person or Zoom Video Option Included. 2nd – On the Date of Your Treatment Included. |
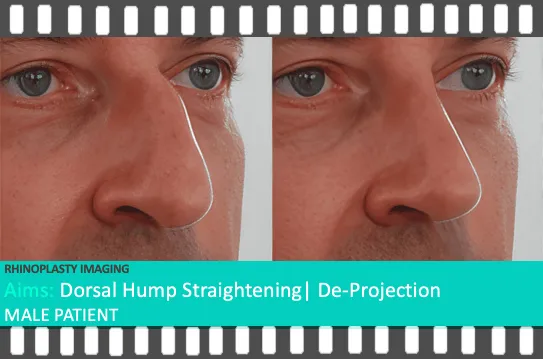
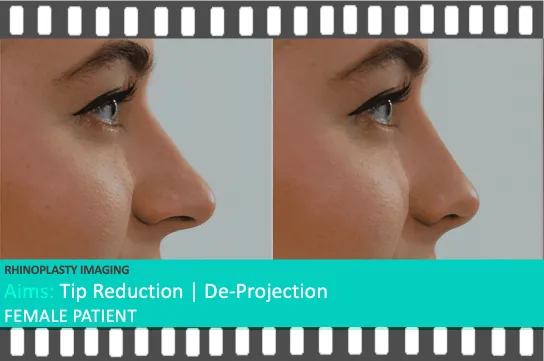
 | Rhinoplasty Imaging Gallery:Front, Angle and Side Profile Gallery of the Predictive Visual Aim of Your Rhinoplasty Treatment Included. |  | Pre-Operative Tests:The Pre-Operative (MRSA) Nasal Swab Test, Essential for Ensuring Safety Before Your Surgical Procedure Included. |
 | Hospital & Anaesthetic Fees:All Hospital Fees, Private Room, Dedicated Nursing Team Assigned For Your Stay Included. |  | Take Home After Surgery:All Medication And Garments Provided To Take Home After Surgery Fully Included. |
 | Complimentary Chauffeur Home:Complimentary Chauffeur Drive Home After Surgery In London Included. Options For Living Outside London Included. |  | 24-Hour Care Post Surgery:Online Messaging Service 24 Hrs For The First 14 days After Surgery Aftercare Guidance Included. |
 | Post Operative Reviews:7-Day Post Operative Review Included. 1-3 Month Surgeon Review Included. 6-12 Month Surgeon Review Included. |  | Non-Surgical Aftercare:Any Non-Surgical Nose Contouring Treatments Included. Any Swelling Reduction (Steroid) Treatment Included. |
“Your Revision Rhinoplasty Deserves More Than a ‘Starting From’ Price – Fixed Fees, Uncompromised Care, Trusted by Thousands”
Choosing Revision Rhinoplasty isn’t just about correcting the past; it’s about finally getting it right. And that begins with knowing what you’re walking into. At our clinic, the cost of revision rhinoplasty is fixed at £9,950.00 — with no vague “starting from” prices, no hidden extras, and no surprises. Our patients receive the full care they need: consultant-led surgery in a CQC-accredited hospital, 24-hour medical support during recovery, full aftercare, and even a complimentary chauffeur home if you live in London.
We understand the emotional and physical toll of needing a second surgery. That’s why every step is transparent, every result intentional, and every patient treated with the highest level of care and honesty. Your second rhinoplasty deserves better, and that starts with clear answers, expert hands, and no compromises.
FINANCE PACKAGES / COSMETIC LOANS
We do not provide Cosmetic Financing for Revision Rhinoplasty. When considering this cosmetic surgery, we like to ensure that your surgery cost is transparent and clear to understand. The above cost includes your completed Revision Rhinoplasty procedure with no additional hidden costs.
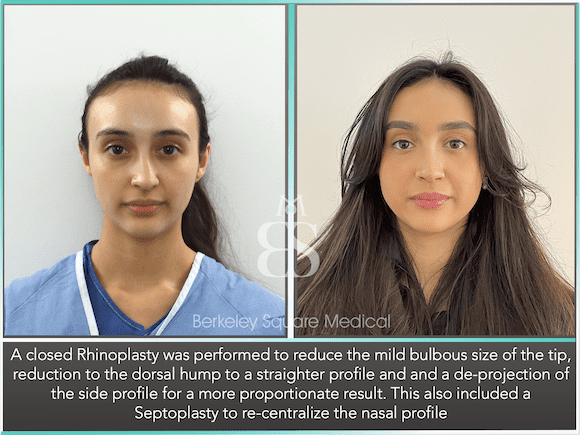
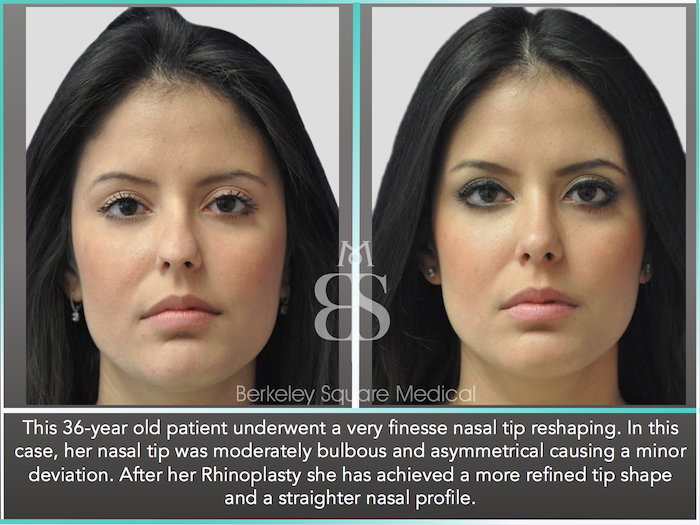
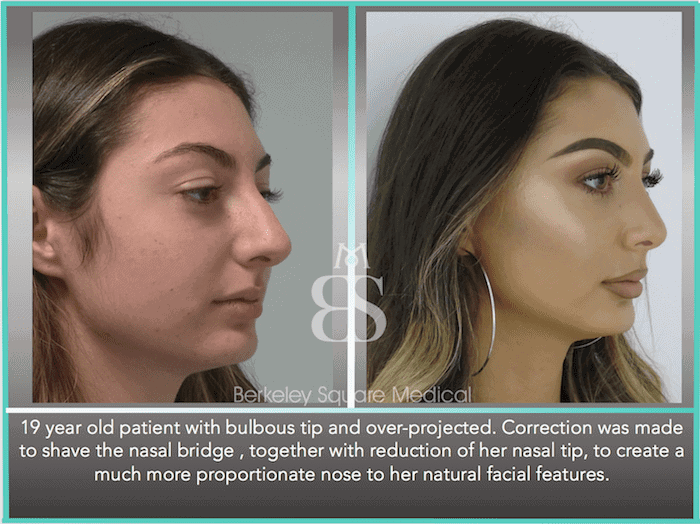
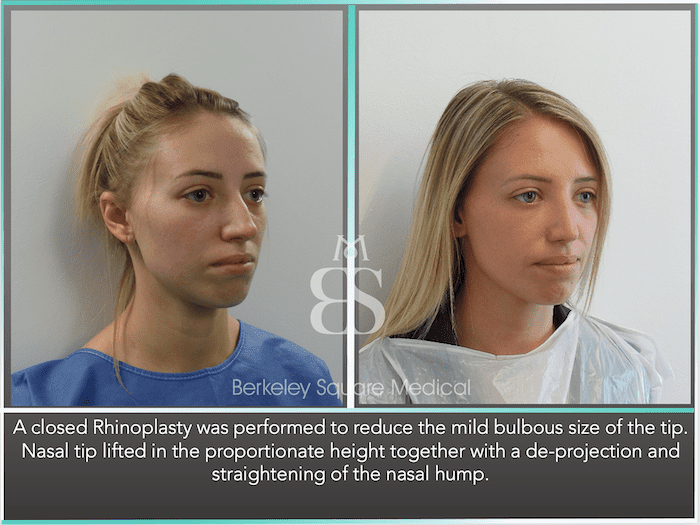
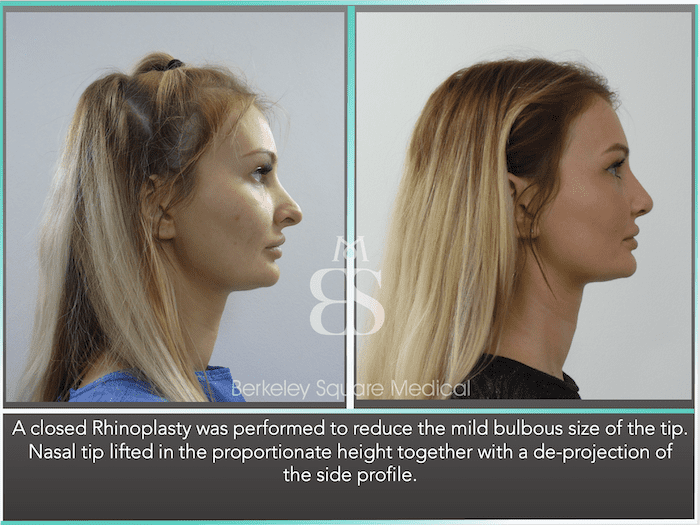
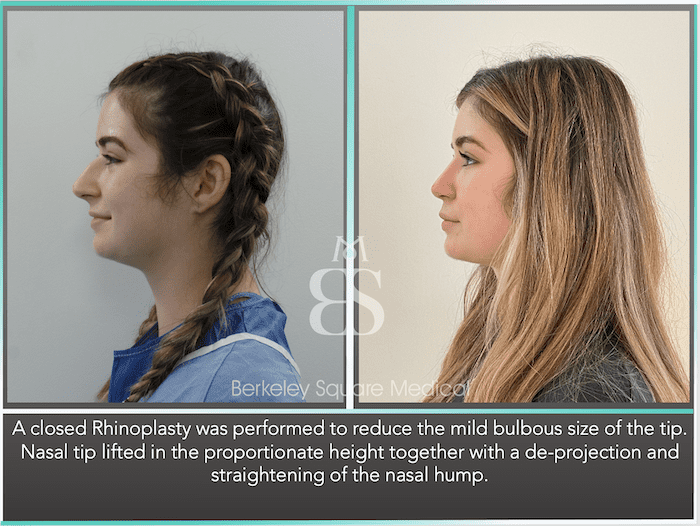
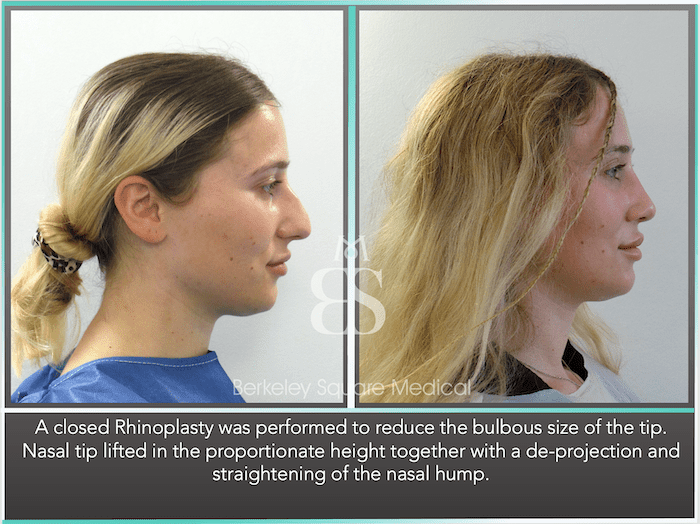
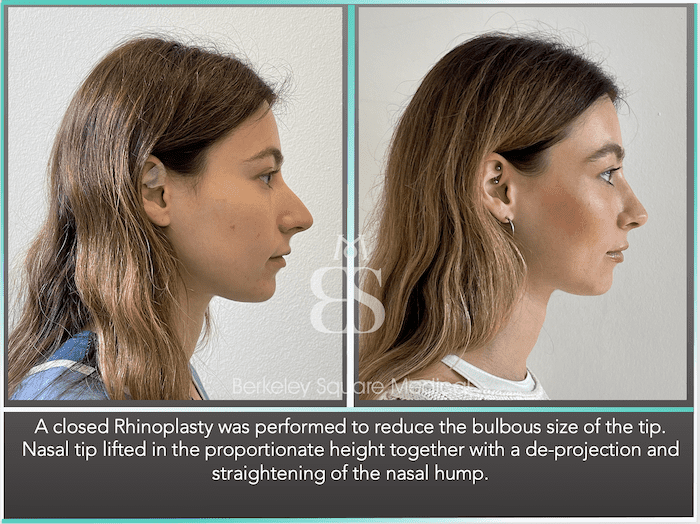
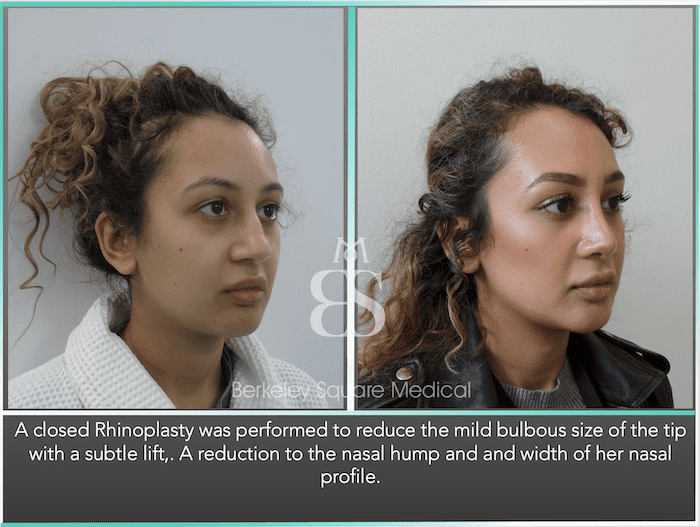
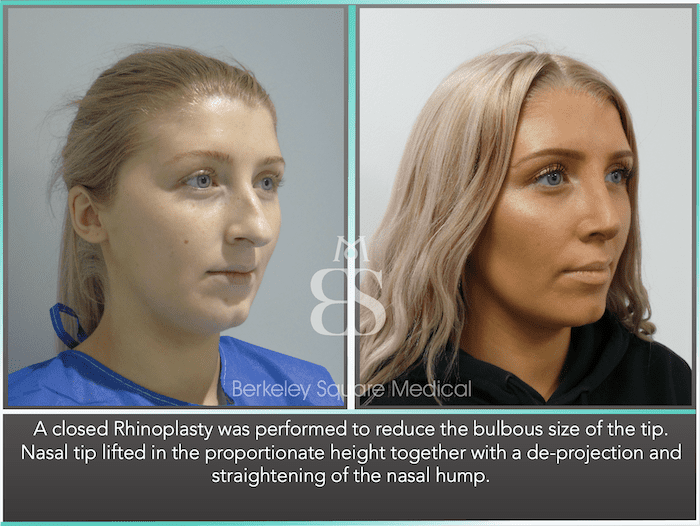
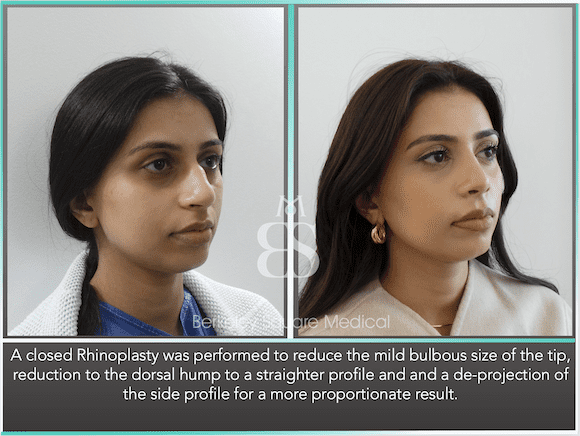
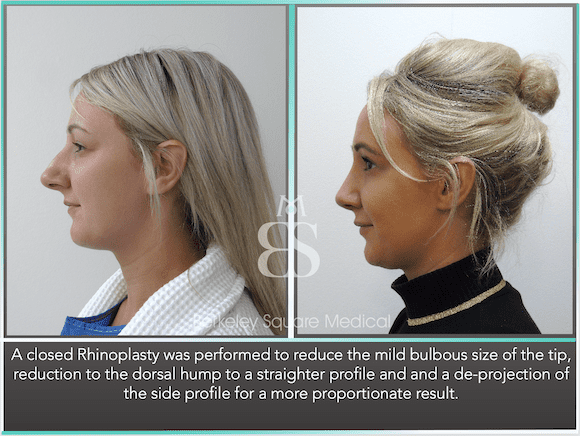
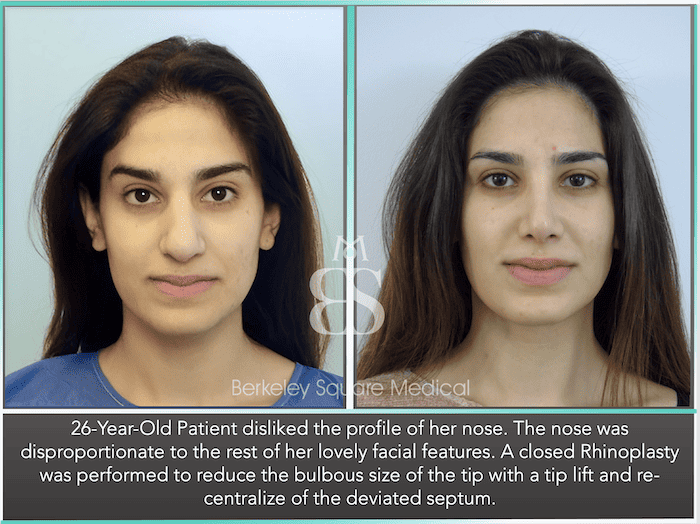
BULBOUS NASAL TIP CORRECTION
- Your Nasal tip requires further reduction to achieve a more proportionate profile.
- You have a build-up of scar tissue from your previous surgery that requires remodelling and reduction.
Your nasal tip sits at the end of your nose, and in some patients, one side of their tip looks different compared to the other. For example, one side may be bigger, smaller, higher, lower, or slightly twisted to one side.
Since the shape of the tip of your nose is largely dependent upon the underlying cartilage, irregular-looking tips usually occur due to your genetics or an injury.
Corrective surgery can be made to the underlying cartilage around the nasal tip so that both sides appear more symmetrical and proportionate.
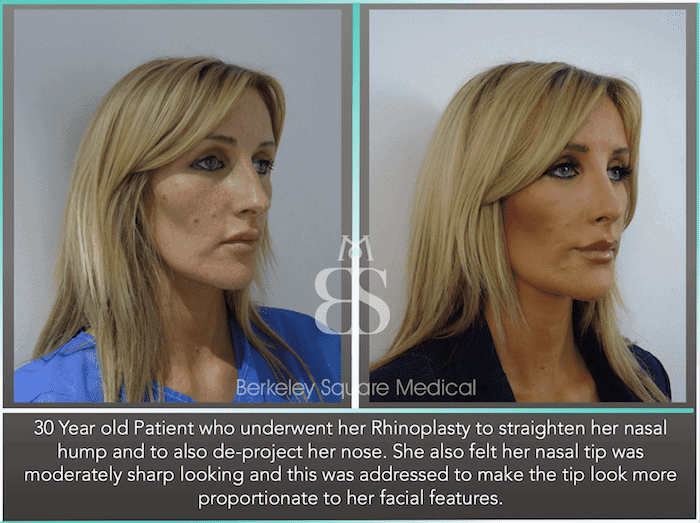
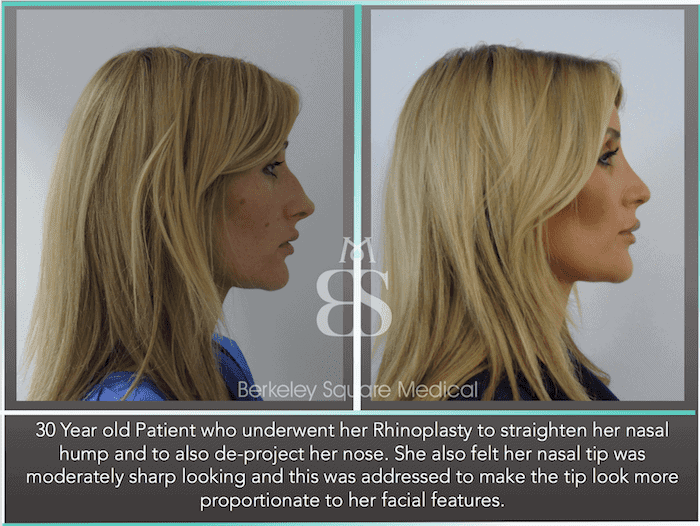
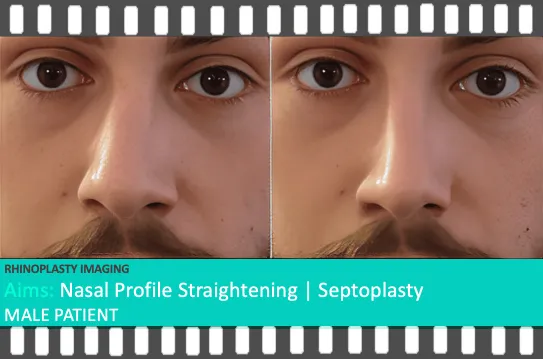
DEVIATED SEPTUM / CROOKED NOSE CORRECTION
- Your nasal bones have not reset correctly, and your nose appears moderately/severely off-centre from your facial features.
- You have a deviated septum that requires straightening to assist with difficulty in breathing.
This procedure is known as a Septoplasty or Septorhinoplasty. Many patients notice that their nose is twisted or deviated, which is more obvious in photos or when natural light reflects their nose.
A crooked nose occurs due to the nasal bones and/or septum that is not centralised down the midline of your facial profile. As a result, the nose leans to one side.
Our Rhinoplasty surgeon will aim to reset the nasal bones and septum to a more central profile.
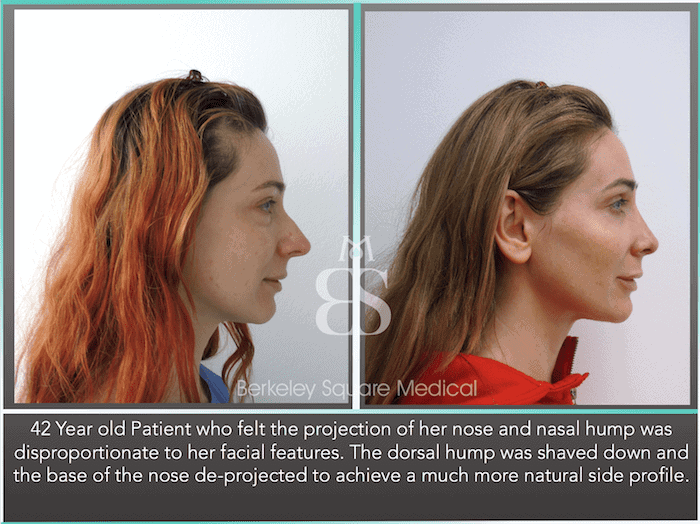
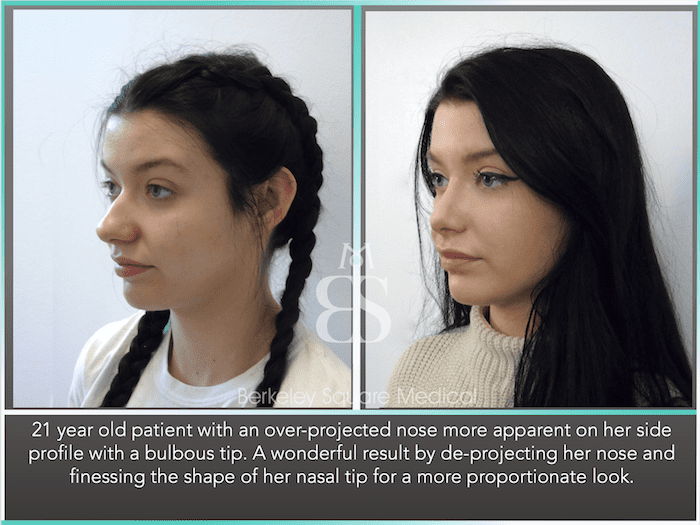
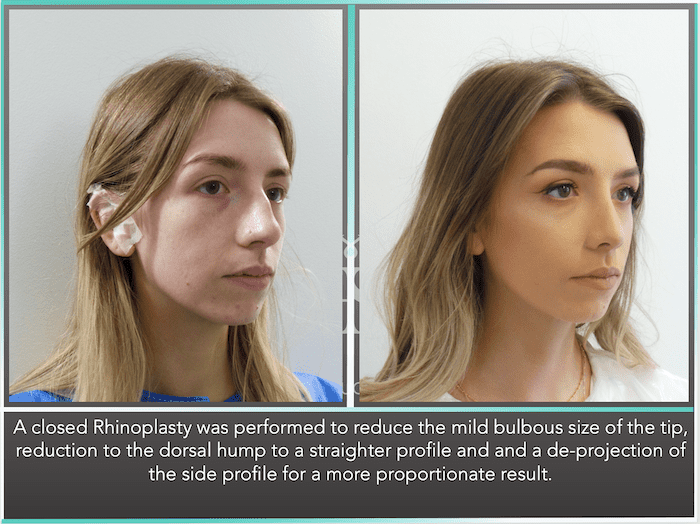
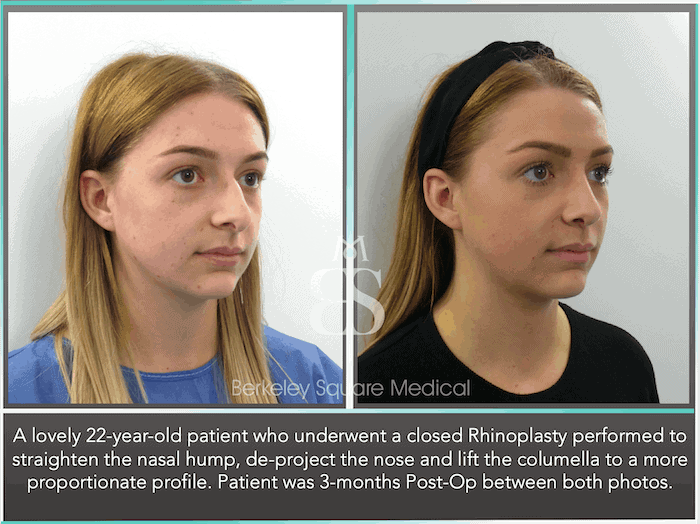
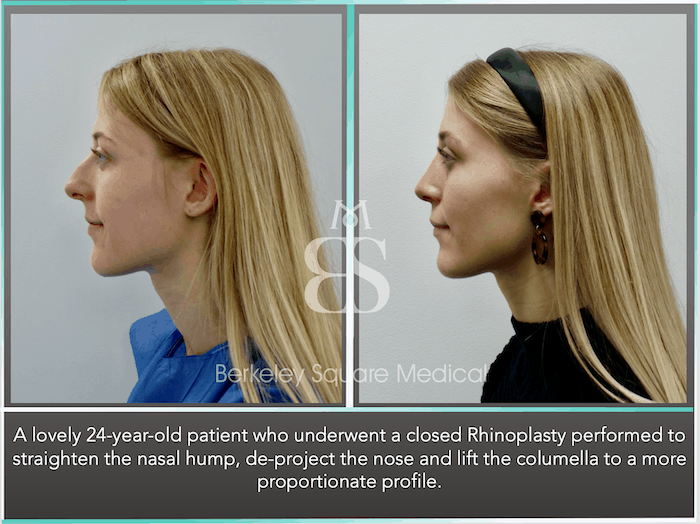
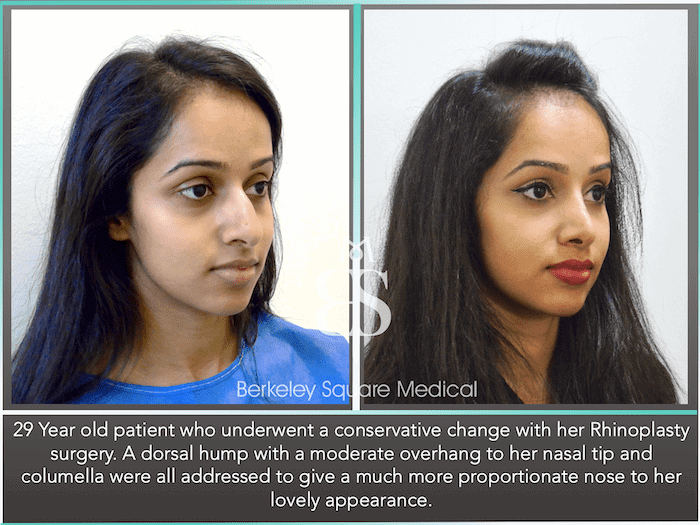
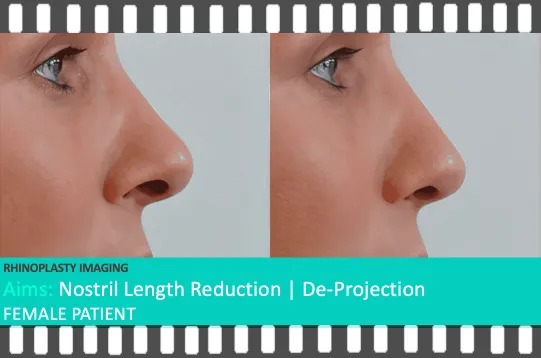
PROJECTED NASAL TIP CORRECTION
- Your nose appears too projected and further away from your upper lip.
- You feel your nose is still too long when viewing your side profile.
Nasal tip projection is a tip that appears to project too far out, so much so that it looks unnatural. When your nasal tip is overly projected, it may also start to hang down towards your upper lip.
There are two ways that a nasal projection can be corrected:
- To reduce the Maxilla Spine of the nose, a thin bone at the base of the nose that gives the nose its projection.
- The second involves reducing the nasal tip cartilage to de-project the nose.
In some cases, both techniques are performed to proportionate your nasal profile.
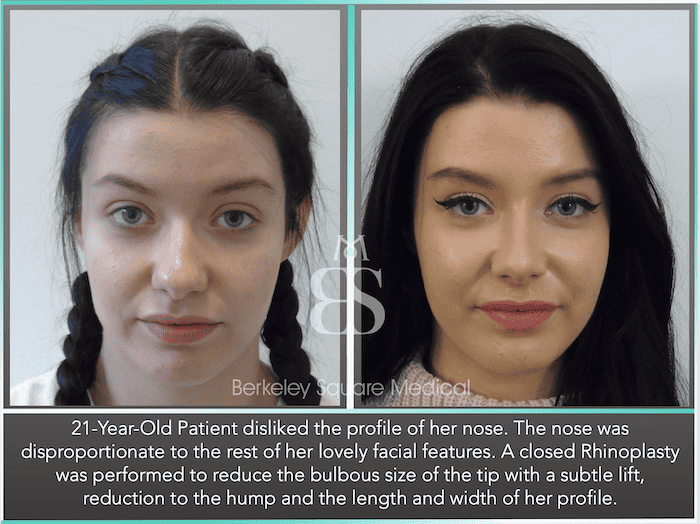
WIDE NOSE CORRECTION
- Your nose is wider after your Rhinoplasty and requires narrowing of the nasal profile when viewing your front-facing profile.
- Your previous surgeon has widened your nose to treat a previous breathing difficulty.
Some people feel their nose looks fine from the side but not from a front-facing profile.If you have a wide nose, several factors will determine the type of results you can expect from revision rhinoplasty surgery.
If your nose is wide due to its underlying bone structure, then the aim is to make a reduction in the width of your nose.
If you have thicker nasal skin, a surgeon can change your nasal shape and make it slightly more narrow, but there may be limitations to how narrow your nose will appear. Thicker-skinned patients in Rhinoplasty often have limits to how much reduction they can achieve in their nose reshaping results. We often advise skin-thinning creams to use before and after surgery to reduce the thickness of the nasal skin, if this is the case.
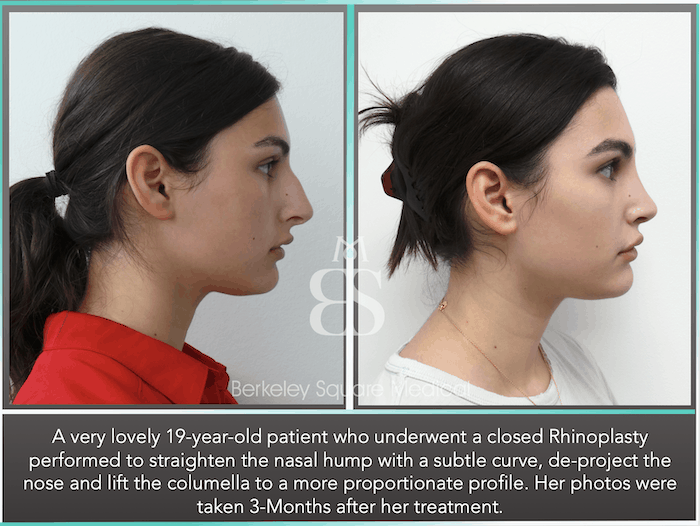
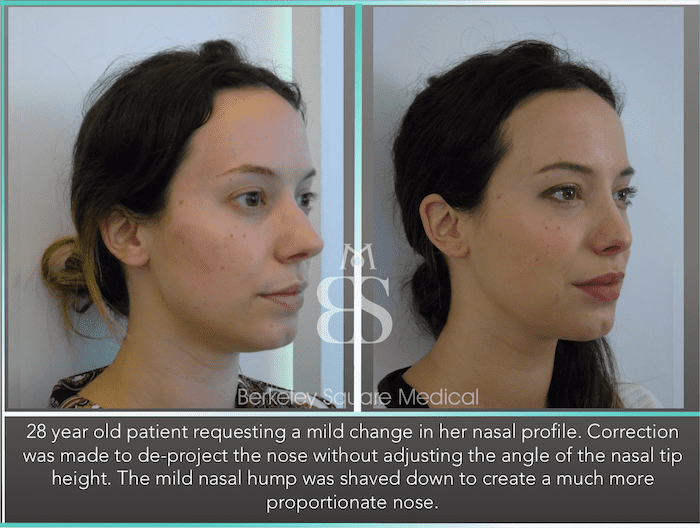
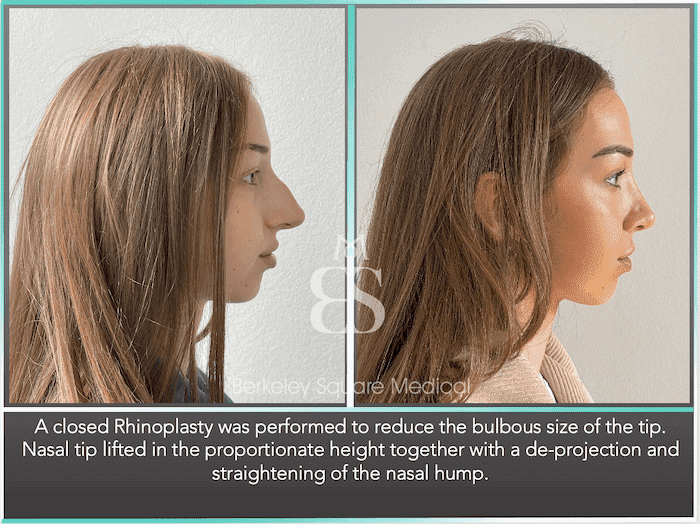
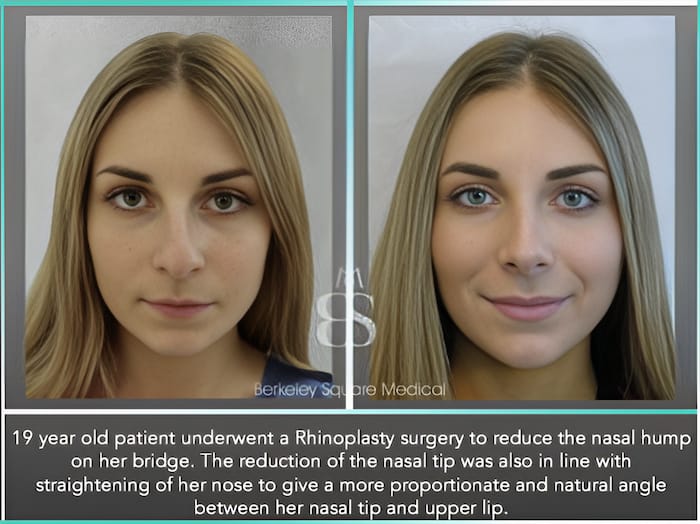
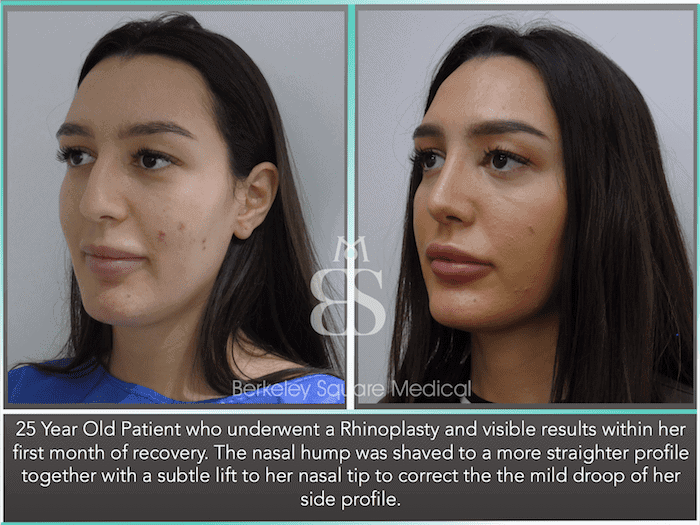
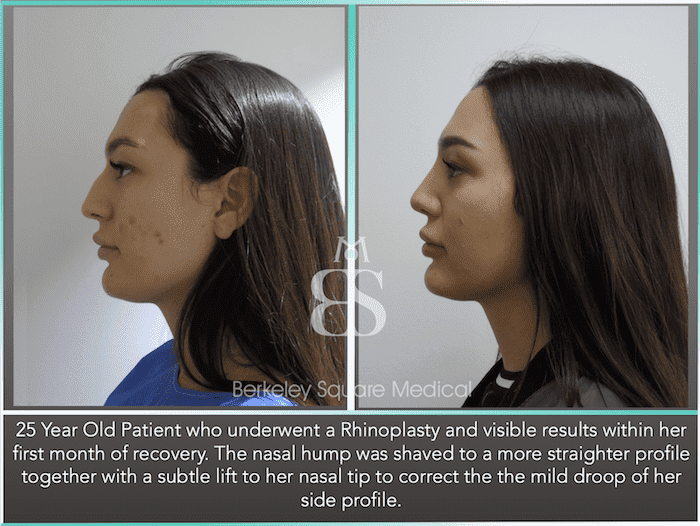
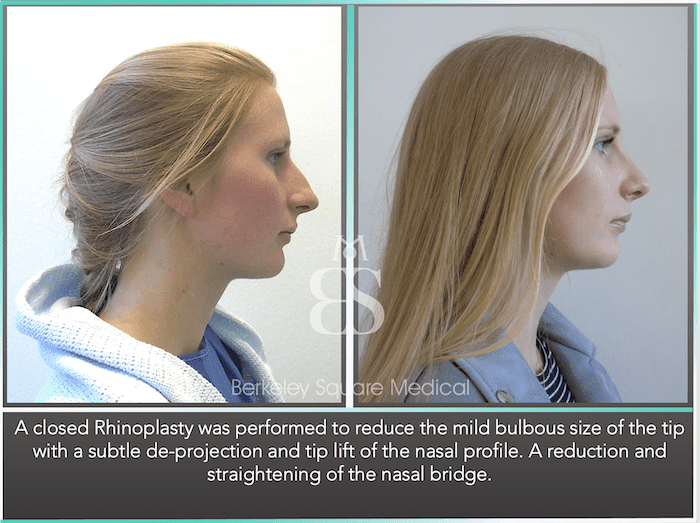
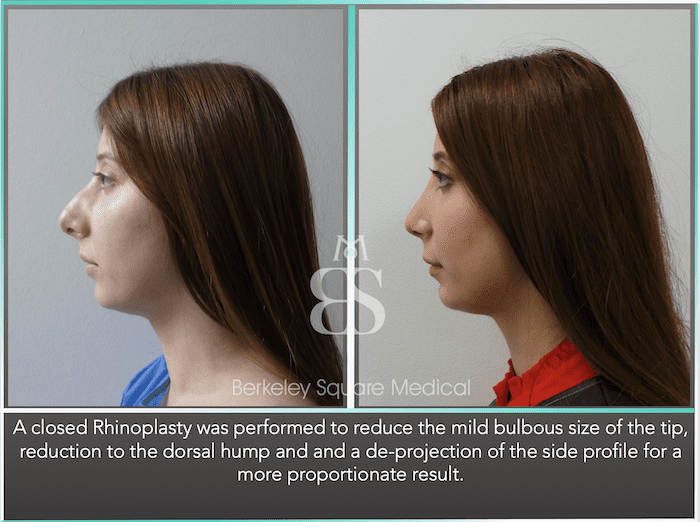
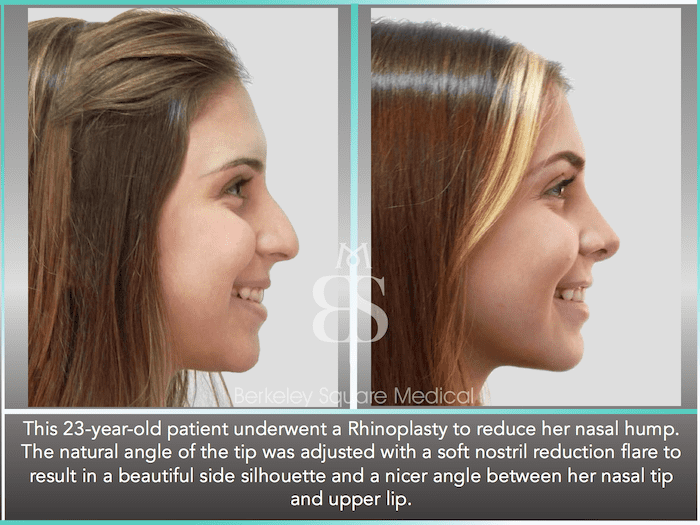
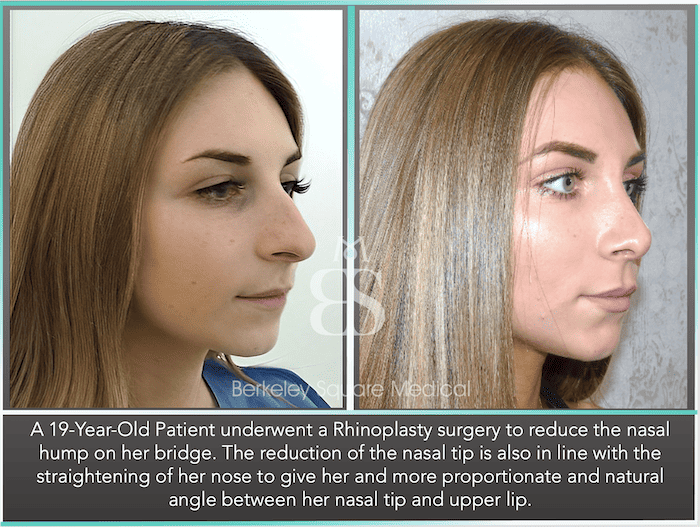
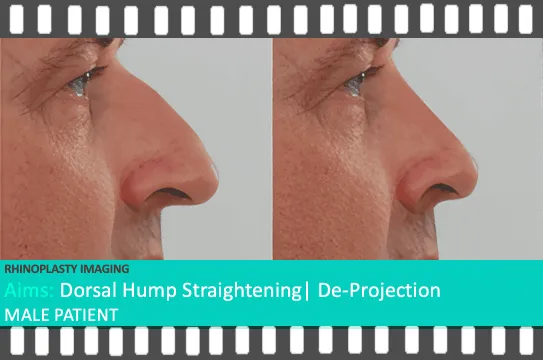
NASAL HUMP CORRECTION
- Your nasal bone is not straight.
- There are minor dips or bumps in the side profile of your nose.
Although your previous surgery aim was to shave and straighten your nasal hump, one of the consented risks of rhinoplasty is dips and bumps to the nasal bone that affect the straightness of your side profile as your bones fully heal.
In almost all cases, this can be corrected by re-rasping the nasal bones without the need for fracturing the bone, which is the cause of this risk in rhinoplasty.
In some instances, patients may also want a very subtle curve to their nasal bridge, and we will advise this at your consultation to ensure this looks natural.
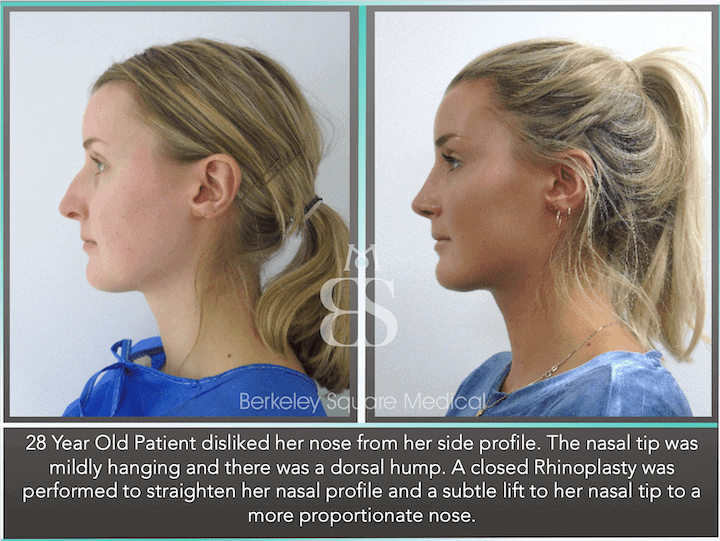
DROOPING NOSE TIP CORRECTION
- Your nasal tip appears bulbous.
- Your nasal tip appears to hang downwards.
Causes of this can be due to the weight of the nasal tip, and reducing the size of the tip / assessing the scar tissue internally from your previous surgery may elevate the tip to a more proportionate angle. In some cases, you may have swelling in the supra-tip cartilage,e causing a bend that requires specialisation to correct.
WIDE OR FLARED NOSTRILS (ALAR BASE REDUCTION)
- Your nostrils remain flared when you smile.
- Your nostrils are asymmetrical.
- Your nostrils appear wider due to the reduction of your nasal tip.
Incisions can be made between the inner nostril and columella (skin between your nostrils) and then brought together to shorten the width of your nostrils. This has to be performed to ensure your breathing channels are not disrupted.
If you previously underwent an Alar Base Reduction as a part of your first surgery, there is an increased chance that further reduction may not be advisable.
If you are considering revision surgery, it is a very important decision to make with your Surgeon. Your consultation will include fully discussing your goals and examining if a secondary rhinoplasty will benefit you before making any corrections. Should you be considering revision surgery, it is important that you obtain a full copy of your previous surgeon’s notes to bring to your consultation with us.
Your consultation is to have a more precise idea of what you can achieve with your cosmetic Rhinoplasty surgery.
Your facial plastic surgeon will first listen to your concerns and would like to fully understand what aspects of your nose are affecting your self-confidence. We also want to know how it is affecting you and to set realistic expectations. This leads your consultation towards the changes you wish to make before your surgeon advises the steps that can be taken with a Rhinoplasty surgery to a successful nose reshaping.
This is a part of your journey where you can decide whether this procedure is right for you and understand the expertise of your surgeon in how he will achieve the best results for you. We aim for proportion to the nose, which ultimately means we aim for a natural final shape for you.
The consultation with your surgeon is:
- To fully discuss what makes you unhappy about your primary rhinoplasty results and what changes you wish to achieve with your revision rhinoplasty.
- To discuss your expectations and then consult you about what can be achieved, keeping within the boundaries of a safe and successful change.
- Conduct an examination of the nose, including the thickness and elasticity of your nasal skin, and light reflection against your nose to observe any minor anomalies in the previous recovery.
- Explain the full procedure in detail to you and the surgical techniques that will be used to help achieve your goal successfully.
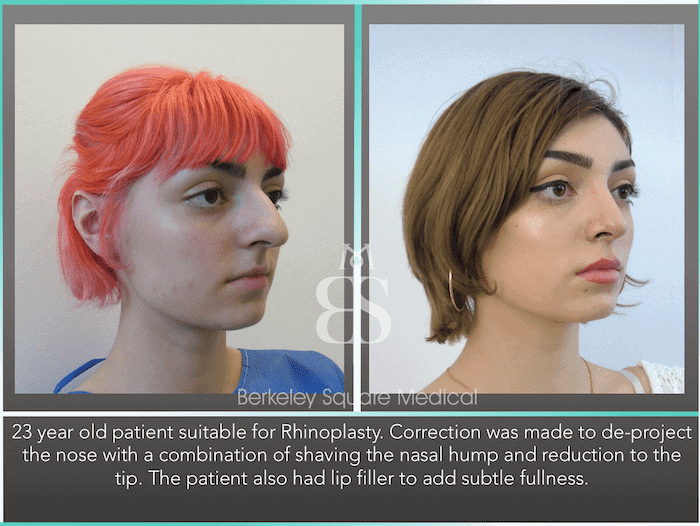
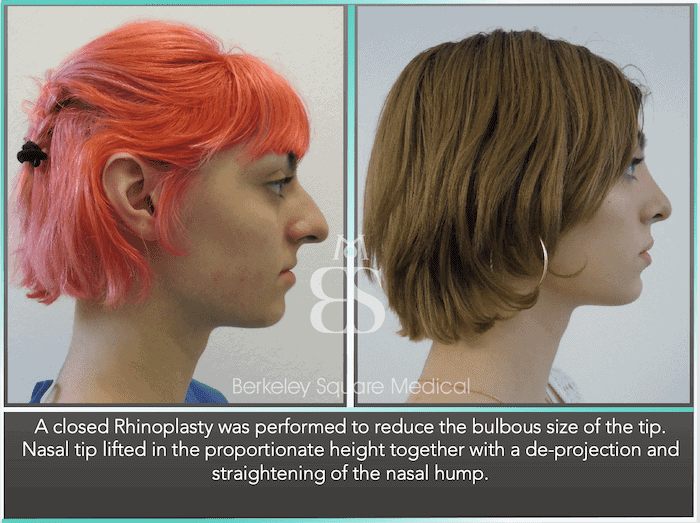
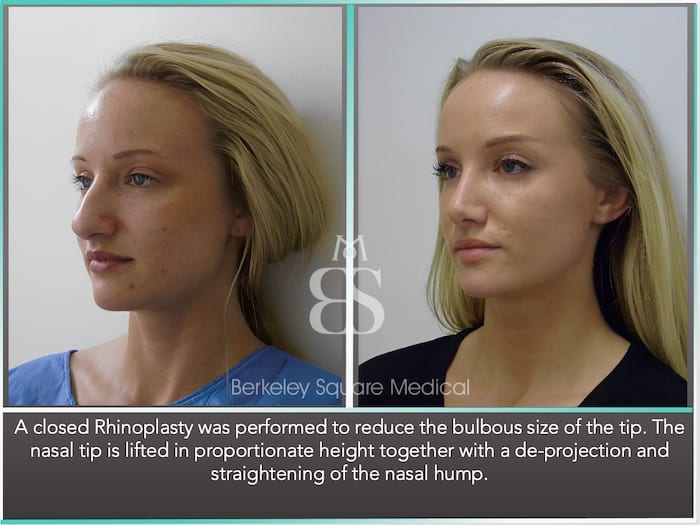
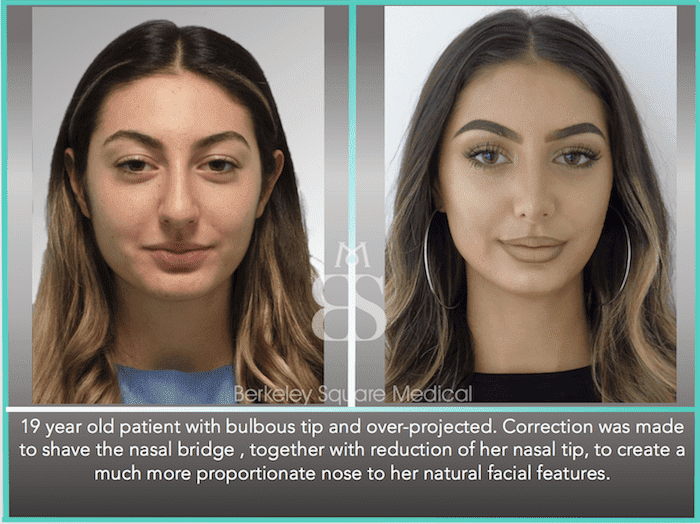
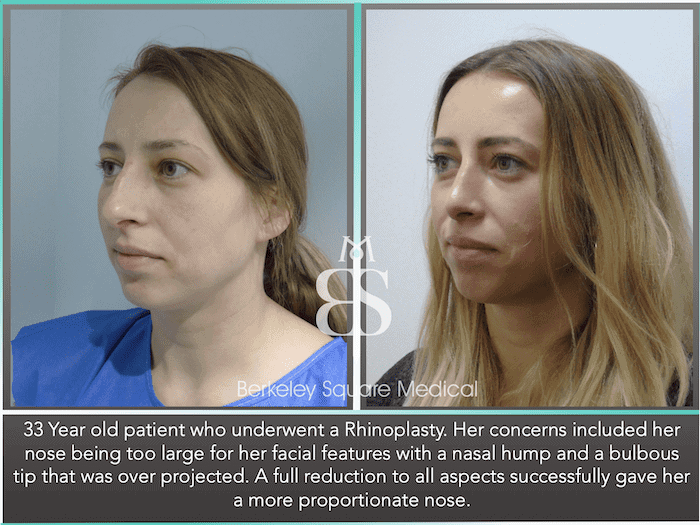
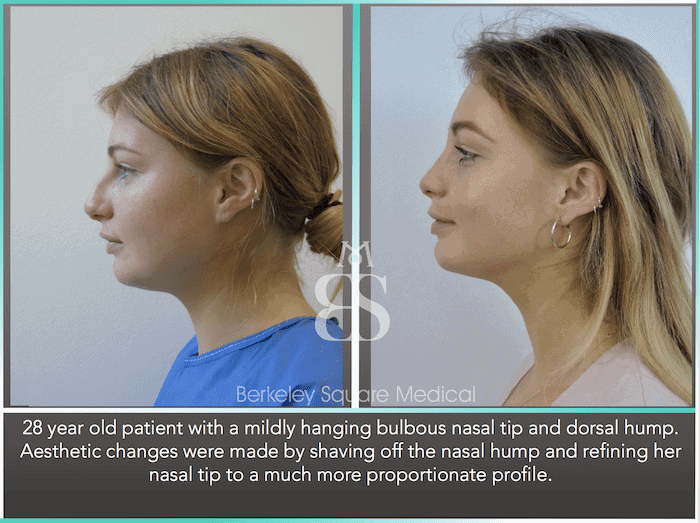
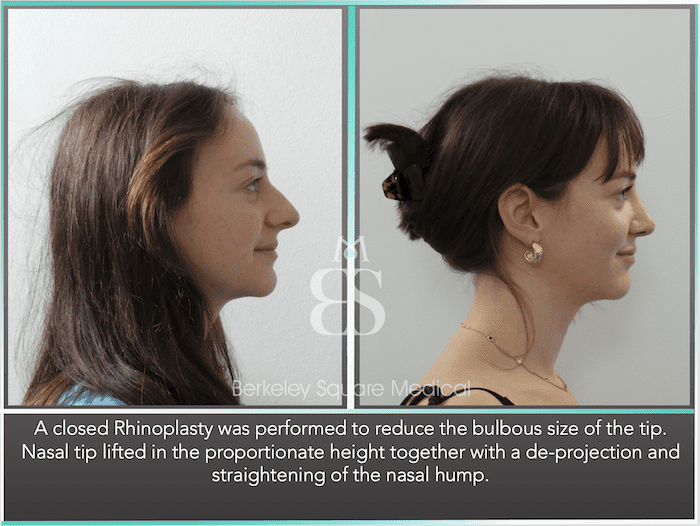
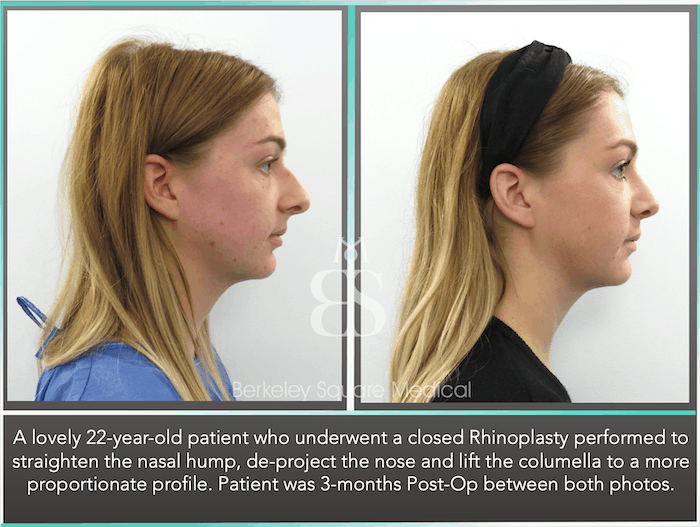
- If applicable, take you through before and after photos of previous patients that best relate to you and the final results other patients have achieved.
- Discuss the risks and benefits associated with a revision surgery, your medical history, and any questions you may have for your Surgeon.
- Advise whether having a preview of your final result with our Rhinoplasty Imaging Service will assist you in making the best decision with your surgeon.
Upon your initial consultation, a second appointment with our Rhinoplasty clinical team will follow, which will provide the confirmed procedure cost, the booking process, and information to take home to read before making an informed decision to have your procedure with us.
We like to provide complete details about our Surgeon’s Accreditations and Awards, more information about our London hospital, and several guidebooklets that guide you through the risks and benefits of nose surgery and the terms and conditions of your treatment.
The surgical techniques used in your corrective surgery will depend largely on the goals desired by you and our Rhinoplasty surgeon. Generally, specialist surgeons prefer to perform all of the incisions inside your nose, where scarring will not be visible.
Below are the two main techniques of nose reshaping surgery that can be performed. Knowing these techniques will make you much better prepared when seeing your surgeon. Both techniques will have advantages and disadvantages relating to your goals, and our surgeon may talk you through these before you decide on the best technique for you.
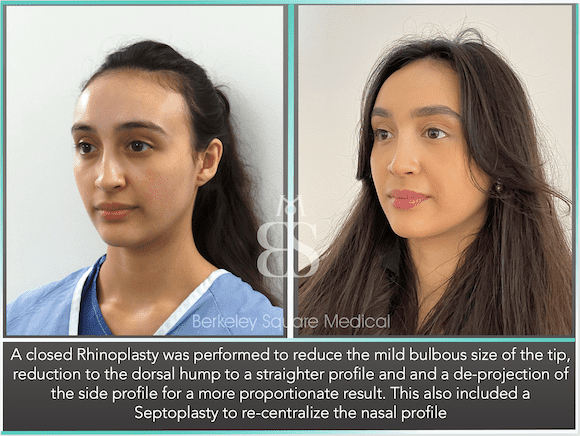
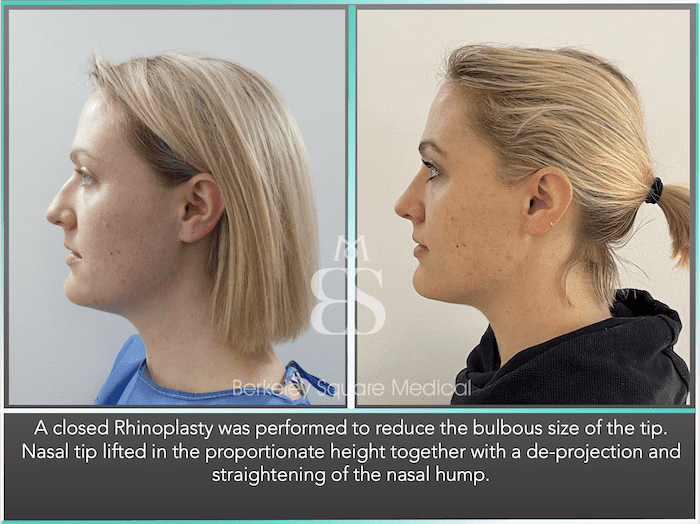
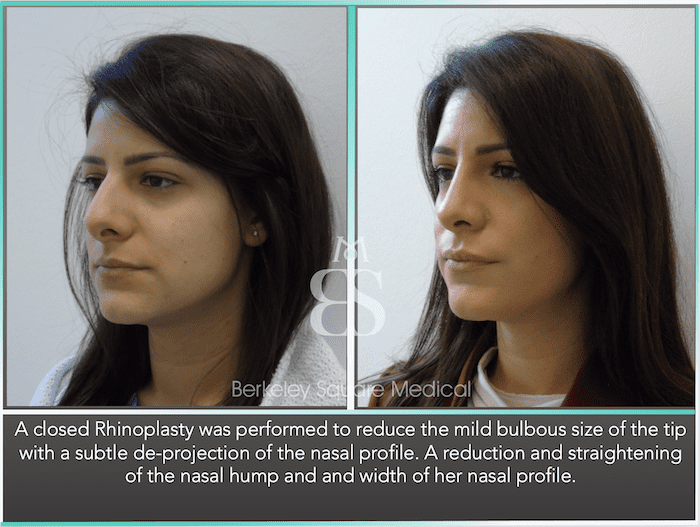
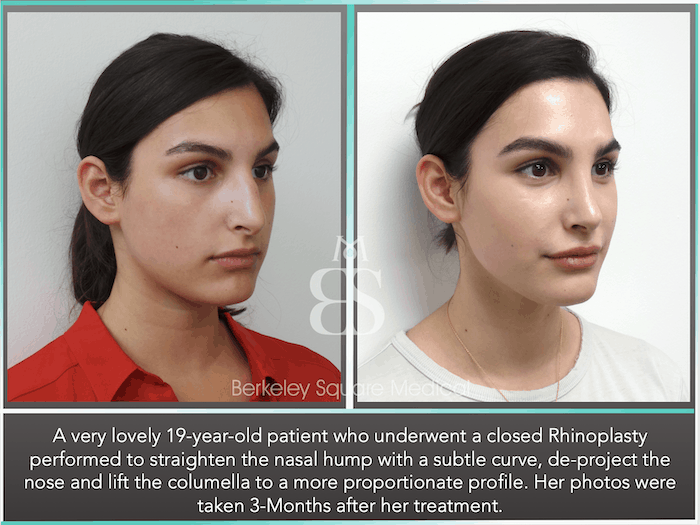
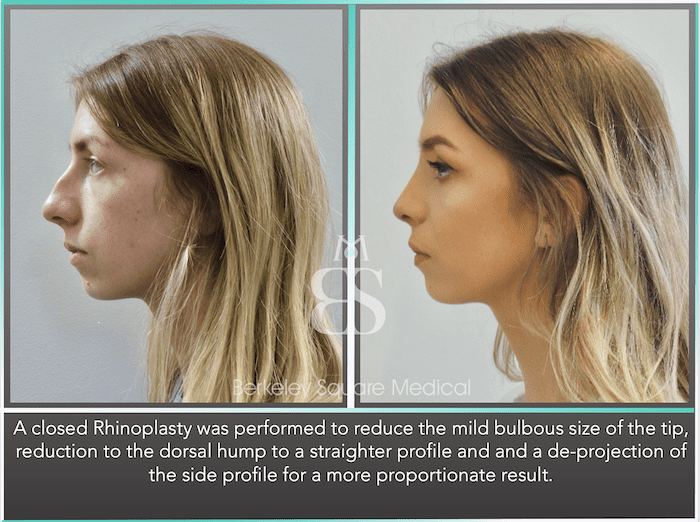
CLOSED RHINOPLASTY
The closed technique is considered a very advanced cosmetic surgery method in the UK and the US and is a technical approach we advise in the first instance. This involves making incisions internally within the nose and has the advantage of leaving no visible external scars. This remains our first choice in approach on all first-time rhinoplasty procedures and many revision cases we treat from other clinics.
Closed rhinoplasty surgery can be used for some types of rhino tip surgery, removing bumps or humps, reshaping cartilage and bones, broken nose cosmetic surgery, deviated septum surgery, preservation rhinoplasty, and removing excess soft tissue.
Ideally, you should elect to have closed rhinoplasty as your first option. This, however, may not be possible in every case, depending on the type of result that you would like to achieve.

OPEN RHINOPLASTY
Open rhinoplasty involves an incision across the lower or mid-columella, the skin in the middle of your nose that sits between the nostrils.
These open incisions allow a surgeon to lift the skin upwards and over your nasal tip, thereby exposing the cartilage and bone structure of your nasal cavity under the soft tissues.
Open rhinoplasty surgery tends to be most suitable for patients undergoing complex procedures such as revision or reconstructive surgery (using cartilage grafts), where clear access to your nasal skeleton is preferred by rhinoplasty surgeons.
You are likely to have a small scar across your columella once you have recovered from your surgery, but in most cases, this scar will fade and be barely visible.
Nose surgery procedures are usually performed under local anaesthesia, but in some cases, total intravenous anaesthesia may be needed.

We are one of very few clinics in the UK to provide direct Online Messaging Services 24 hours a day with 2 dedicated members of our rhinoplasty clinical team who are on hand to assist you during your recovery, as well as your Surgeon.
BEFORE YOU LEAVE OUR HOSPITAL
Our priority is that your rhinoplasty recovery process is straightforward and quick. You will be provided with aftercare instructions by our surgeon and nursing team once ready to be discharged from the hospital. This will include any pain medications and antibiotics (if applicable). All nasal packs are removed completely before you leave the hospital.
We want to ensure that you can get home safely. For this reason, all rhinoplasty patients are chauffeur driven home complimentary (Within London/Greater London) as a part of our aftercare to you.
THE FIRST 24 HOURS AFTER SURGERY
You will feel slightly tired from the general anaesthetic medication until it wears off. You may also be generally exhausted from the experience of a long day; at this point, any swelling to the nose will increase, together with a blocked nose. Slight breathing difficulties are expected. Bleeding may also continue slightly within the first 24 hours, and padding is provided to absorb any slight discharge.
THE FIRST 3 DAYS AFTER SURGERY
Patients feel much better after the first and second day after the nose job, with more energy and a sense of returning to normal indoor activities. Bruising and swelling reach their maximum point within the first 72 hours, and you may notice you are more swollen than when you left the hospital on the day of your cosmetic surgery.
Pain and discomfort are generally mild and can be managed with over-the-counter medication. Most patients report that breathing from their mouth creates the most discomfort, but no pain.
5 DAYS AFTER SURGERY
Generally, the healing process is well underway, and all patients will see a significant improvement in swelling and bruising. Bruising discolouration has subsided and turned yellow, and swelling has noticeably reduced.
7 DAYS AFTER SURGERY
You will return to the hospital for your first post-operative review, in which any stitches are removed together with your nasal splint. We often tell our patients to soak their nasal splint the night before their appointment to make removing it pain-free.
Though our surgeons use dissolvable skin sutures, we will check to ensure your incisions have healed. You will also be assessed for any leftover swelling and any advice to help improve your rhinoplasty recovery time. Any international patients can travel by air at this point (unless otherwise agreed to depart earlier).
8-10 DAYS AFTER SURGERY
Your nose may slightly widen 24 hours after removing your nasal splint, but this usually resolves back to normal within 24-48 hours. Your nose will start to take a better shape, and although you will still have tip swelling, you will undoubtedly notice the change in shape and size of your nose. You can start to resume very light gym and cardio in moderation. Most patients will return to work at this stage in recovery with no signs that a surgical procedure has occurred.
1 MONTH AFTER SURGERY
Your nose will be improving in shape and size. It is advisable to monitor progress on a 6-weekly schedule instead of a daily observation. This helps patients take the attention off their noses and gives a greater sense of calmness during the recovery.
3 MONTHS AFTER SURGERY
You will have been booked for your second post-operative appointment with our dedicated nursing team or Surgeon. This appointment is to evaluate the initial results and recovery progress, including:
- Taking your first set of post-operation photos
- Comparing your pre-surgery and initial post-surgery photos
- Assessing how your bones are healing and swelling reduction, and where we expect further reduction and change.
- Advisingon any treatments that we may want to perform or recommend to help with your recovery for both aesthetic and functional purposes.
6 MONTHS AFTER SURGERY
Your third post-operative appointment with be around the 6-month stage. This review is much like the 3-month review, but a continuation of observing your nose, which will be closer to its final result, and assessing the finesse differences between your 3-month recovery photos and the new photo gallery on this day.
1 YEAR AFTER SURGERY
As a part of your aftercare, we advise all patients to book around their anniversary stage for a final assessment of the results. The full recovery after a nose reshaping surgery takes up to 12 months, but can sometimes continue with minor internal healing. This is because we include all the hidden aspects of the recovery, such as inner cartilage scar healing and superficial swelling reduction.
Revision Rhinoplasty Recovery and Risks: A Personalised Approach by Mr Taimur Shoaib
Revision rhinoplasty is one of the most technically demanding procedures in facial plastic surgery. Unlike a first-time (primary) rhinoplasty, a revision involves correcting or rebuilding what has already been operated on, often in the presence of scar tissue, weakened cartilage, and unpredictable healing patterns. The stakes are naturally higher, but so too is the importance of experience and judgement.
Mr Taimur Shoaib has performed hundreds of complex revision rhinoplasty procedures, many of which involved correcting work carried out by other surgeons. His approach is deliberate, honest, and built on a guiding principle: he will not undertake revision surgery if the risks outweigh the achievable aesthetic or functional outcome. Revision rhinoplasty is not about chasing perfection — it’s about restoring balance, form, and confidence with care and precision.
The Recovery Journey: What to Expect After Revision Rhinoplasty
Recovery after revision rhinoplasty follows the same general structure as a primary procedure, but is often slower and more nuanced. The tissues have already been altered, which means:
- Swelling takes longer to resolve, especially at the nasal tip.
- Healing is less predictable, particularly where scarring or previous grafts are present.
- Skin may not redrape as easily, especially if it has thinned from prior surgery.
Most patients return to desk-based work or light activity within 10–14 days. However, visible refinement of the nose can take 12 to 24 months, particularly in complex cases. This timeline reflects the delicate process of the nose re-settling and the skin adapting to the underlying framework.
At every stage, Mr Shoaib remains closely involved in monitoring your recovery. You will be seen regularly, especially in the first few months, to assess healing and address any concerns early.
Understanding the Risks — And How They Differ from Primary Rhinoplasty
No surgery is without risk. However, in revision rhinoplasty, the potential for complications is higher due to altered anatomy and existing scar tissue. Some of the key risks include:
1. Persistent or Worsening Asymmetry
In revision cases, asymmetry can be harder to correct because the natural tissue planes have been disrupted. Scar tissue can also “pull” the nose during healing.
Mr Shoaib mitigates this by meticulously evaluating where the asymmetry originates from — skin, cartilage, or bone — and addresses each layer separately during surgery.
2. Breathing Difficulties
Structural support may be compromised from the previous surgery, especially if too much cartilage was removed.
In such cases, Mr Shoaib may use cartilage grafts, often harvested from the ear or rib, to rebuild and support the nasal airway. His goal is not only an aesthetically improved nose but one that functions properly.
3. Unpredictable Swelling and Scar Tissue Formation
Scar tissue is more aggressive in revision cases and can obscure results for many months.
Where necessary, Mr Shoaib may use gentle steroid injections in the months following surgery to soften internal scar tissue and allow the nasal contours to become more defined over time.
4. Over-Correction or Under-Correction
Each revision carries a tighter margin for change, and sometimes a nose may be limited in how much it can be improved without risking long-term harm.
This is precisely why Mr Shoaib will turn patients away if he feels the structure cannot withstand further surgery — or if the improvement would be marginal and not justify the risk.
The Role of Follow-Up and Aftercare
After your surgery, Mr Shoaib will remain actively involved in your recovery:
- Scheduled follow-ups take place over a 12–24 month period.
- Ongoing photographic assessments help track changes in subtle ways.
- Steroid management is used when appropriate to control scar-related swelling.
- Breathing assessments are made throughout recovery if functional issues were addressed.
By maintaining a close relationship with each revision rhinoplasty patient, Mr Shoaib ensures the healing process aligns with the original plan, and that no issue is left unattended.
Revision rhinoplasty is not a procedure to be rushed or taken lightly. It demands experience, restraint, and a willingness to say “no” when necessary. Mr Taimur Shoaib’s commitment to these principles is what sets his work apart — not just in London, but across the UK.
If you are considering revision rhinoplasty, know that the decision to operate must be based on anatomy, not just emotion. A well-timed, well-planned revision can restore confidence, but only when it is in the right hands — and for the right reasons.